CRISPR’s Potential Beyond Gene Editing
Since its discovery, CRISPR (“Clustered Regularly Interspaced Short Palindromic Repeats”), which won the 2020 Nobel Prize in Chemistry, has revolutionized medicine and biotechnology.
Source: Nobel Prize
This is because CRISPR is the first method for gene editing that allows for very precise targeting of a specific genetic sequence, allowing for correcting genetic errors either in vitro or in vivo without risking unwanted mutations.
This is important as undirected gene insertion has been linked to major problems, notably cancer risks, making their therapeutic use difficult and controversial.
CRISPR can be used in multiple ways to interrupt a gene already present, delete a specific sequence, or edit/insert the right genetic sequence.

Source: CRISPR Therapeutics
This turned into a medical breakthrough with the FDA approval for the first CRISPR-based therapy in 2023, developed by CRISPR Therapeutics (CRSP -2.25%) for genetic blood diseases (follow the link for a dedicated report about CRISPR Therapeutics).
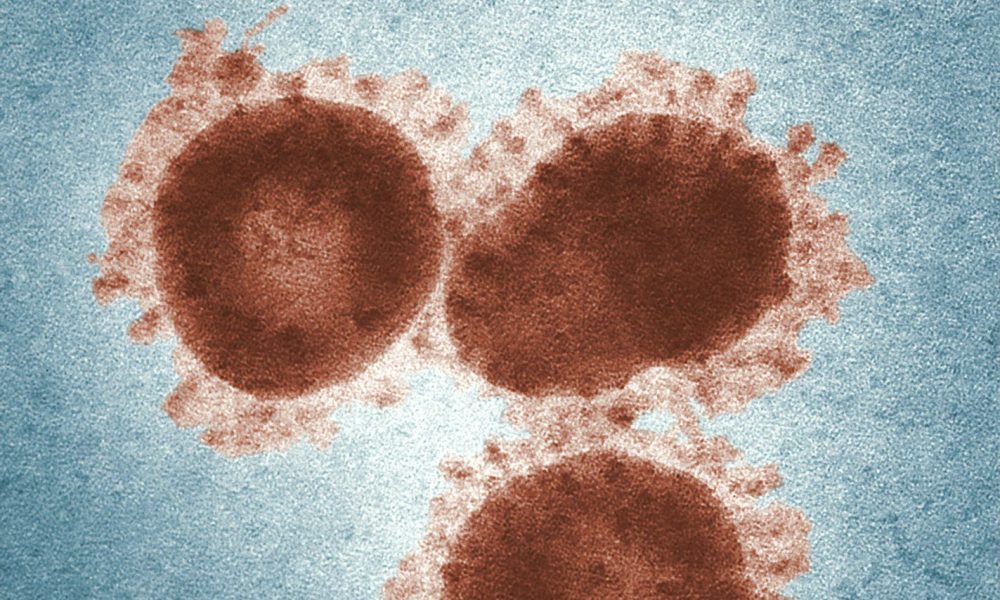
However, human-controlled precise gene editing is not what CRISPR was used for in nature. This is, first and foremost, an antiviral tool that bacteria use to survive attacks from viruses.
So this raises the question if CRISPR could be used in the same fashion to treat human viruses. Especially the ones that are the hardest to fight with vaccines or antiviral treatment.
This is the idea investigated by researchers at the Islamic Azad University (SRBIAU) (Iran), Semnan University of Medical Sciences (Iran), Shahid Beheshti University of Medical Sciences (Iran), Shahroud University of Medical Sciences (Iran), and University of Bergen (Norway).
They published their findings in a systematic review of ongoing research in the field in MDPI, under the title “Progress in CRISPR Technology for Antiviral Treatments: Genome Editing as a Potential Cure for Chronic Viral Infections”.
The Natural Origins of CRISPR as a Viral Defense
Most bacteria are under constant threat of viruses specialized in attacking them, called bacteriophages (literally named “bacteria eaters”). Phages work by landing on the bacteria, and injecting it with its genetic material, to replicate more viruses.

Source: Innovative Genomics
Each CRISPR genetic sequence found within an individual bacterial CRISPR is derived from a DNA fragment of a bacteriophage that had previously infected the prokaryote or one of its ancestors.
This way, the CRISPR system can recognize the bacteriophage genetic material, and cut it in pieces before it manages to reproduce into new virus particles.
This forms a sort of “acquired immunity” for bacteria against phage viruses. CRISPR is found in approximately 50% of sequenced bacterial genomes.
Considering how widespread CRISPR systems are, and how important they are against viral infections for bacteria, could such a method be used to treat viruses in humans too?
Targeting Chronic Infections With CRISPR
Why Chronic Infections?
When discussing viral infection, chronic infections are the prime concern for doctors. This includes viruses like HIV or hepatitis.
An issue specific to these diseases that allows them to elude both treatment and the body’s immune system is that they can go dormant, with the viral genetic material embedded in the cell, sometimes silent for years.
Sometimes, the provirus switches to an inactive mode that cannot be transcribed, which raises an issue.
Not only can the human immune system not attack these latent reservoirs, but the antiretroviral medications also fail to act upon these non-transcribing sections. Some of these HIV-1 reservoirs can survive for up to 60 years in CD4+ T cells.
There are a few ways CRISPR technology could be used to target these chronic viral infections.
Can CRISPR Help Cure HIV/AIDS?
One option is through genetic engineering, to create human cells that are missing the receptors required for the viral infection to work. In the case of AIDS/HIV, modified immune CD4+ T cell without the CCR5 & CXCR4 co-receptors become resistant to the virus and can block its entry.
This approach seems to work in the lab but will require extensive animal studies and then human trials to determine if it is efficient and safe enough to become a reliable cure for the disease.
The same method of modifying the human cells is considered for hepatitis C. CRISPR-Cas13a targeting the entry site of the virus into liver cells prevents the virus replication effectively with extremely limited damages to the liver cells, much lower than the ones caused by the virus.
CRISPR vs. Dormant Hepatitis B Infections
Similar to HIV, the hepatitis B virus forms a latent viral reservoir using “covalently closed circular DNA” (cccDNA) in liver cells.
Studies in cultured cells indicated that CRISPR systems targeted against conserved sequences in the hepatitis B genome can successfully reduce 98% of hepatitis B’s DNA material.
Fighting HPV With CRISPR
Human papillomavirus, or HPV, is a sexually transmitted virus that can cause precancerous lesions that later on can turn into cancer, not only in the cervix but also in other organs. It, too, can become dormant.
Some vaccines for HPV exist, but do not cover all the types of HPVs, and cannot help with preexisting infections.
CRISPR systems can upregulate pRb, a host tumor-suppressor protein, blocking the growth of positive HPV cells and inhibiting their cancerous activity.
Using CRISPR to Address Epstein–Barr Virus (EBV)
Epstein–Barr virus, or EBV, is a virus that infects immune cells (lymphocytes B) and causes infectious mononucleosis, while sometimes it can develop into malignant cancers, like Burkitt’s lymphoma.
Here, too, modifying the immune cells can block their evolution toward cancer, effectively suppressing the worst effects of EBV.
CRISPR vs. Traditional Antiviral Approaches
As we saw with the recent COVID pandemic, a recurring issue for vaccines is how to target a part of the virus that is stable and constant enough between strains for the vaccine to stay effective despite quick mutations.
This is because viruses are very good at modifying their surface proteins, the only ones accessible to antibodies created by the vaccines.
In contrast, CRISPR-Cas13d-based methods can target conserved genetic sequences coding for the capsid protein and RNA polymerase, which are necessary for the virus proliferation.
By focusing on these conserved areas, PAC-MAN aims to deliver broad-spectrum efficacy against various virus strains and even across related viruses.
The same method could be used for flu viruses, which are even more able to mutate constantly and evade existing vaccines.
For example, up to 92% of known influenza A strains were successfully targeted with just six crRNAs, and similar success was achieved with SARS-CoV-2 using 22 crRNAs.
CRISPR Antiviral Therapies: Future Outlook and Limitations
Even if the CRISPR system is able to adapt to mutation, this is not entirely foolproof, as the continuous adaptation of bacteriophages to natural CRISPR systems proves. So while these methods might prove a big medical progress, it is unlikely to be a silver bullet either.
Off-target modification of the human genome is also a risk, especially with CRISPR-Cas9 systems, which can eventually cause mutation or toxicity of the treatment. This has been less of a concern for gene therapy of deadly genetic diseases without any cure, leading to the recent approval of these gene therapies.
For infectious diseases in larger populations, the FDA may take a harder line and more cautious approach, slowing down the path to commercialization of these therapies.
The delivery system of the CRISPR system into the host cells is also not trivial. Viral vectors or nanoparticles can create unwanted immune reactions or target other organs than the desired ones.
Progress in CRISPR therapy, from using other versions than Cas9 (like CRISPR-Cas12a), or new vectors more tolerated by the human body, will also benefit the progress of CRISPR antiviral therapies.
In addition, new methods like using Cas13, which target viral RNA without harming the host DNA, are especially suitable for a rapid response against RNA viruses like SARS-CoV-2.
Investing in CRISPR Innovation
Editas
Editas Medicine, Inc. (EDIT -6.48%)
Editas was founded by CRISPR-Cas9 co-discoverer Jennifer Doudna. Editas started working with Cas9 but is now focused on a proprietary version of Cas12a that they engineered: AsCas12a.
You can read more about Cas12a’s unique properties in our dedicated article “What Is CRISPR-Cas12a2? & Why Does It Matter?”.

Source: Editas
You can also read an overview of all of Jennifer Doudna’s companies in the corresponding article “Top Jennifer Doudna Companies to Watch.”
Editas is focused on Sickle Cell Disease (SCD) and beta-thalassemia, 2 diseases where it lost the race for first treatment approval to competitors CRISPR Therapeutics and BlueBirdBio.
Overall, the SCD program (recently renamed Reni-Cell) has been delayed several times, sparking concern among investors, and has since been refocused on in vivo therapy to distinguish it from already approved SCD therapies.
Nevertheless, Editas owns significant patents on CRISPR-Cas12, which has been used by researchers at the University of New South Wales, Australia, to develop a COVID-19 strip test, illustrating the technology’s potential beyond gene editing.
Editas also signed in 2023 a $50M deal with Vertex for the company to use Editas’ Cas9 IP.
Editas focuses on other CRISPR versions than the “classical” CRISPR-Cas9 and its research IP might come in handy in establishing partnerships and generating revenues without an FDA-approved product, on top of a cash runway going into 2026.
As Cas12a seems to become increasingly proven as a best-in-class method for multi-gene editing, Editas’ expertise and pipeline focus on this CRISPR variant might prove a winning bet in the long run.
(You can read more about CRISPR companies in our corresponding article “Top 5 CRISPR Companies To Invest In”.)
Latest Editas (EDIT) Stock News and Developments
Studies Referenced:
1. Nouri, F., Alibabaei, F., Forouzanmehr, B., Tahmasebi, H., Oksenych, V., & Eslami, M. (2025). Progress in CRISPR Technology for Antiviral Treatments: Genome Editing as a Potential Cure for Chronic Viral Infections. Microbiology Research, 16(5), 104. https://doi.org/10.3390/microbiolres1605010